Headaches in Children: A Parent's Guide
Comprehensive guide for parents on recognizing, understanding, and managing headaches in children. Learn about pediatric headache types, warning signs, when to seek help, and effective home management strategies.
Headaches in Children: A Parent’s Guide
As a neurologist with extensive experience in both the UK and India, I’ve helped countless families understand and manage headaches in children. Through my practice and work with SAMMAN, I’ve seen how early recognition and proper management can make a significant difference in a child’s well-being, academic performance, and overall quality of life.
Understanding Headaches in Children
In my practice, I’ve observed that headaches in children are more common than many parents realize:
- Prevalence: Headaches affect approximately 10-20% of children
- Increasing Frequency: Headaches become more common as children grow older
- Impact: Can significantly affect school performance, social activities, and family life
- Early Recognition: Important for effective management and prevention
Why Do Children Get Headaches?
Based on my clinical experience, children can develop headaches for various reasons:
Common Causes
- Tension Headaches: Often related to stress, school pressure, or poor posture
- Migraines: Can be triggered by various factors including foods, sleep, or hormonal changes
- Sinus Headaches: Related to allergies or infections
- Eye Strain: From excessive screen time or uncorrected vision problems
- Dehydration: Not drinking enough fluids
- Skipping Meals: Irregular eating patterns
- Sleep Issues: Too little or too much sleep, irregular sleep schedule
Less Common Causes
- Underlying Medical Conditions: Infections, head injuries, or other health issues
- Medication Side Effects: Some medications can cause headaches
- Environmental Factors: Bright lights, loud noises, strong smells
- Hormonal Changes: Especially during puberty
Recognizing Headache Types in Children
Through my work with families, I’ve found it helpful for parents to understand different headache types:
Tension Headaches
- Description: Dull, aching pain, often described as a tight band around the head
- Frequency: Most common type in children
- Duration: Can last from 30 minutes to several days
- Triggers: Stress, anxiety, poor posture, eye strain
- Symptoms: Usually no nausea or vomiting, mild sensitivity to light or sound
Migraines in Children
- Description: Moderate to severe throbbing pain, often on one side
- Frequency: Affects about 5-10% of children
- Duration: Typically 1-72 hours
- Triggers: Foods, sleep changes, stress, hormonal changes
- Symptoms: Nausea, vomiting, sensitivity to light and sound, may have aura
- Special Features: Children’s migraines may be shorter, bilateral, and may not have all typical symptoms
Sinus Headaches
- Description: Pain in forehead, cheeks, or around eyes
- Frequency: Less common than tension headaches
- Duration: Varies with underlying sinus condition
- Triggers: Allergies, infections, weather changes
- Symptoms: Nasal congestion, runny nose, facial pressure
Cluster Headaches
- Description: Severe, intense pain, often around one eye
- Frequency: Rare in children
- Duration: Short but very intense attacks
- Triggers: Not well understood
- Symptoms: Eye redness, tearing, nasal congestion on affected side
Warning Signs: When to Worry
Through my years of practice, I’ve identified these critical warning signs that require immediate medical attention:
Emergency Symptoms
- Sudden, Severe Headache: Especially if it’s the worst headache your child has ever had
- Headache with Fever and Stiff Neck: Possible meningitis - seek immediate care
- Headache After Head Injury: Even minor injuries need evaluation
- Headache with Confusion or Loss of Consciousness: Neurological emergency
- Headache with Weakness or Numbness: Possible stroke or other serious condition
- Headache with Vision Loss: Requires immediate evaluation
- Headache that Wakes Child from Sleep: May indicate increased intracranial pressure
- Headache with Seizure: Neurological emergency
Red Flags Requiring Prompt Medical Attention
- Persistent Vomiting: Especially with headache
- Headache Worsening Over Time: Progressive symptoms
- Headache with Personality Changes: Behavioral changes
- Headache with Balance Problems: Coordination difficulties
- Headache with Speech Problems: Difficulty speaking
- Headache in Very Young Children: Under 6 years old with new headaches
- Headache After Age 5: New onset headaches in young children need evaluation
When to Schedule an Appointment
- Frequent Headaches: More than once per week
- Headaches Affecting Daily Life: Missing school or activities
- Headaches Not Responding to Treatment: Over-the-counter medications not helping
- Headaches with Concerning Symptoms: Any unusual symptoms
- Parental Concern: When you’re worried, it’s worth discussing with a doctor
Common Triggers in Children
Based on my experience with families, these are common triggers:
Lifestyle Triggers
- Stress: School pressure, social situations, family stress
- Sleep Issues: Too little sleep, irregular sleep schedule, oversleeping
- Skipping Meals: Irregular eating patterns, not eating breakfast
- Dehydration: Not drinking enough fluids, especially during activities
- Excessive Screen Time: Prolonged use of computers, tablets, phones
- Poor Posture: Especially during school or screen time
Dietary Triggers
- Caffeine: Found in sodas, chocolate, some medications
- Processed Foods: High in additives and preservatives
- Aged Cheeses: Tyramine content
- Artificial Sweeteners: Aspartame and others
- Food Additives: MSG, nitrates, nitrites
- Irregular Meal Times: Skipping meals or eating at irregular times
Environmental Triggers
- Bright Lights: Fluorescent lighting, bright sunlight
- Loud Noises: Sudden or continuous loud sounds
- Strong Smells: Perfumes, chemicals, smoke
- Weather Changes: Barometric pressure changes
- Allergens: Pollen, dust, pet dander
Hormonal Triggers
- Puberty: Hormonal changes during adolescence
- Menstrual Cycle: In adolescent girls
- Growth Spurts: Physical changes during development
Recognizing Headaches in Young Children
In my practice, I’ve found that very young children may not be able to describe their headaches clearly:
Signs in Preschool Children
- Crying or Irritability: May be the only sign of headache
- Holding Head: Child may hold or rub their head
- Avoiding Activities: May avoid bright lights or loud noises
- Sleep Changes: May want to sleep more or have difficulty sleeping
- Appetite Changes: May not want to eat
- Behavioral Changes: May become withdrawn or aggressive
Signs in School-Age Children
- Complaining of Head Pain: Can describe location and type
- Avoiding School: May try to avoid school due to headaches
- Difficulty Concentrating: May have trouble focusing
- Sensitivity to Light or Sound: May want dark, quiet room
- Nausea or Vomiting: May feel sick with headaches
- Fatigue: May feel tired or weak
Home Management Strategies
From my experience with families, these strategies often help:
Immediate Relief Measures
- Rest in Quiet, Dark Room: Reduces sensory stimulation
- Cold or Warm Compress: Applied to forehead or neck
- Hydration: Encourage drinking water
- Gentle Massage: Neck and shoulder massage if child allows
- Relaxation Techniques: Deep breathing, guided imagery
- Comfort Measures: Favorite blanket, stuffed animal, or music
When to Use Medication
- Over-the-Counter Options: Paracetamol (acetaminophen) or ibuprofen
- Dosage: Use age-appropriate dosing based on weight
- Timing: Give early in headache for best effect
- Frequency: Avoid frequent use (more than 2-3 times per week)
- Consultation: Always consult doctor before regular medication use
- Avoid Aspirin: Never give aspirin to children under 18 (risk of Reye’s syndrome)
Non-Pharmacological Approaches
- Relaxation Techniques: Deep breathing, progressive muscle relaxation
- Distraction: Engaging activities to take mind off pain
- Comfort Items: Favorite toys, blankets, or activities
- Gentle Movement: If child feels up to it, gentle activities may help
- Hydration: Ensure adequate fluid intake
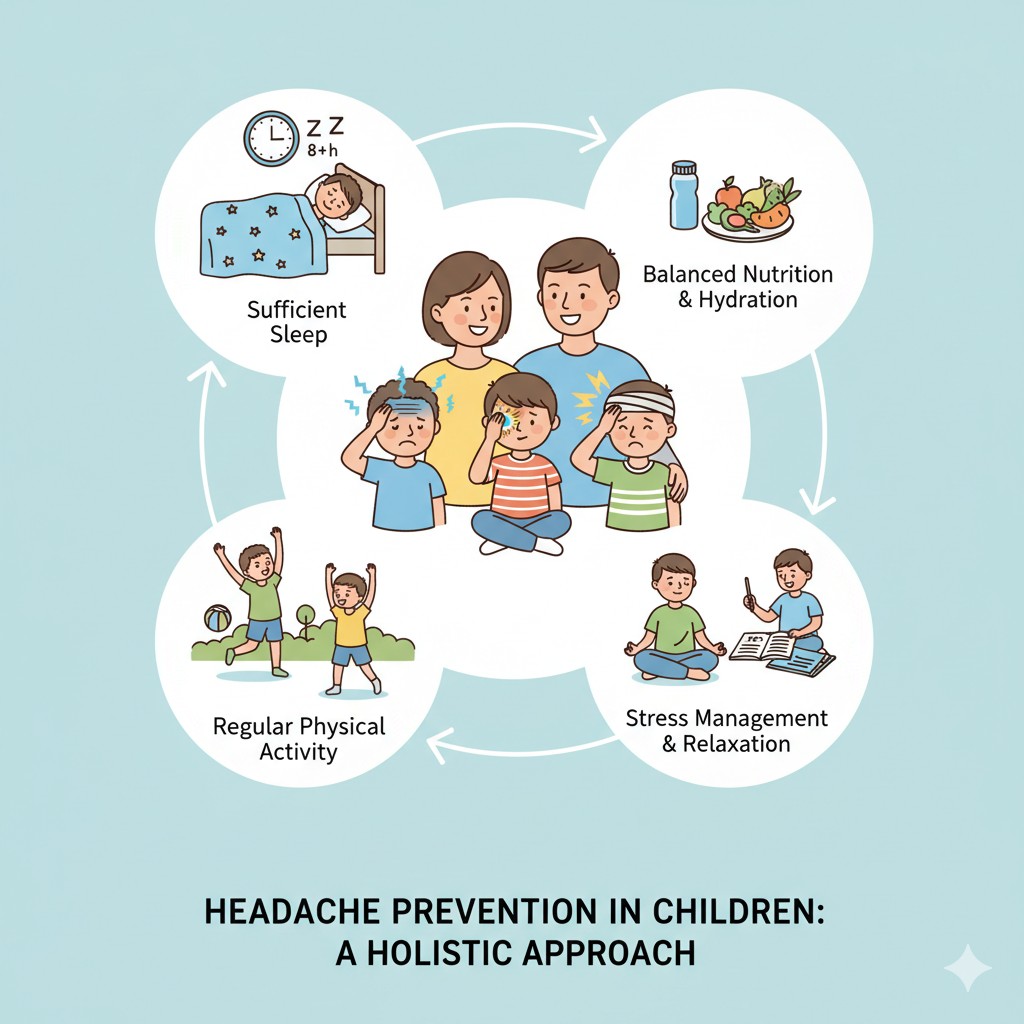
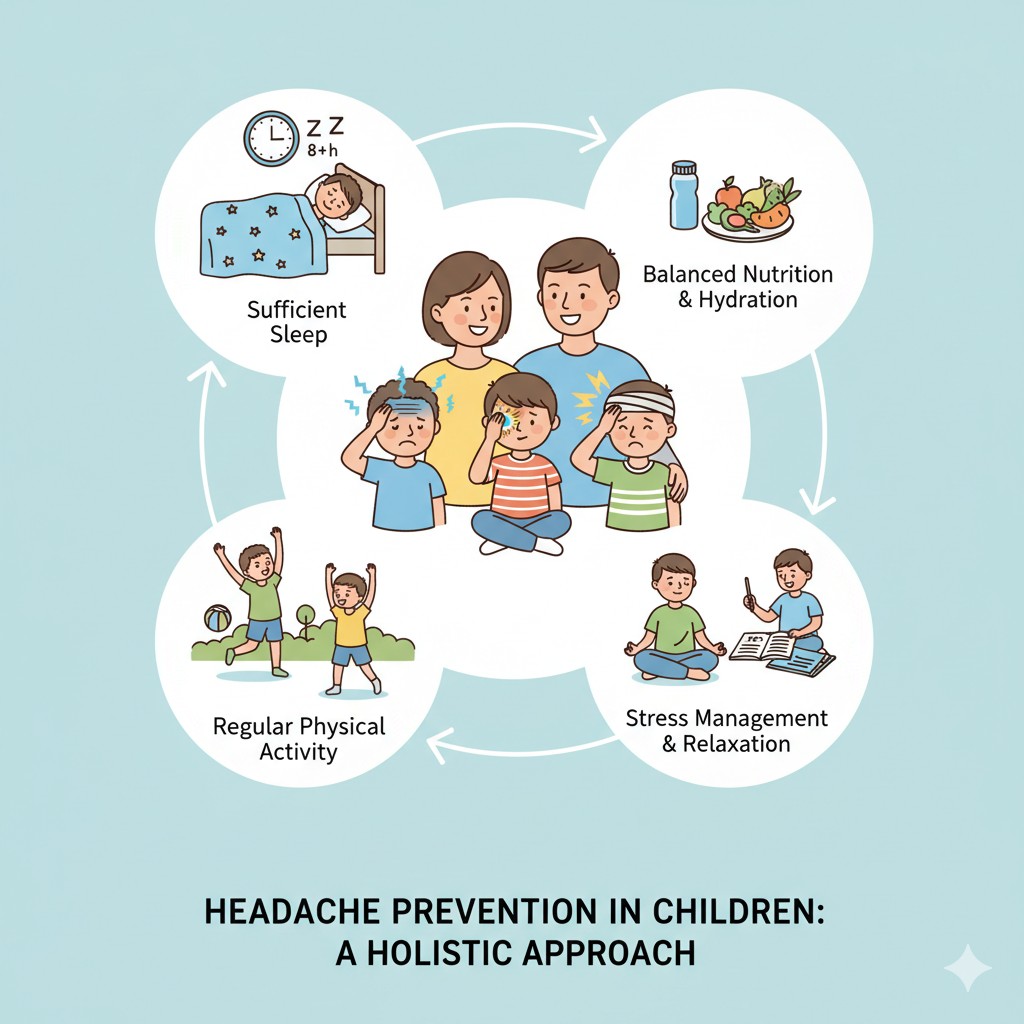
Prevention Strategies
Based on my work with families, these prevention strategies are effective:
Lifestyle Modifications
- Regular Sleep Schedule: Consistent bedtime and wake time, even on weekends
- Adequate Sleep: Age-appropriate sleep duration
- Regular Meals: Consistent meal times, don’t skip breakfast
- Hydration: Encourage regular water intake throughout day
- Regular Exercise: Age-appropriate physical activity
- Screen Time Limits: Reasonable limits on screen use
- Regular Breaks: From screen time and activities
Stress Management
- Open Communication: Encourage child to express feelings
- Stress Reduction: Help identify and manage stressors
- Relaxation Techniques: Teach deep breathing, mindfulness
- Time Management: Help with schoolwork and activity planning
- Support System: Ensure child has support from family and friends
- Professional Help: Consider counseling if stress is significant
Environmental Modifications
- Proper Lighting: Avoid harsh fluorescent lights
- Ergonomic Setup: Proper desk and chair height for schoolwork
- Regular Breaks: From screen time and activities
- Noise Management: Quiet study space when possible
- Allergen Control: If allergies are triggers
Dietary Considerations
- Regular Meal Times: Consistent eating schedule
- Balanced Diet: Include fruits, vegetables, whole grains
- Adequate Hydration: Regular water intake
- Limit Trigger Foods: If specific foods are identified as triggers
- Avoid Skipping Meals: Especially breakfast
School Considerations
In my practice, I’ve found these school-related strategies helpful:
Communication with School
- Inform Teachers: Let them know about child’s headaches
- School Nurse: Ensure nurse is aware and has treatment plan
- Accommodations: Request reasonable accommodations if needed
- Emergency Plan: Have plan for severe headaches at school
- Medication Policy: Understand school’s medication policy
Possible Accommodations
- Flexible Schedule: When possible, flexible start times
- Rest Breaks: Allow rest breaks during school day
- Reduced Screen Time: If screen time is a trigger
- Lighting Adjustments: Seating away from bright lights
- Water Access: Allow water bottle in classroom
- Early Dismissal: For severe headaches when needed
Academic Support
- Missed Work: Plan for making up missed schoolwork
- Flexible Deadlines: When headaches affect ability to complete work
- Alternative Assignments: If screen time is problematic
- Support Services: Access to school counselor or support services
When to Seek Medical Help
Based on my experience, here’s when to consult a healthcare provider:
Schedule an Appointment
- Frequent Headaches: More than once per week
- Headaches Affecting Daily Life: Missing school or activities
- Headaches Not Responding to Treatment: Over-the-counter medications not helping
- New Onset Headaches: New pattern or type of headache
- Worsening Headaches: Increasing frequency or severity
- Parental Concern: When you’re worried, it’s worth discussing
Emergency Care
- Sudden, Severe Headache: Especially worst headache ever
- Headache with Fever and Stiff Neck: Possible meningitis
- Headache After Head Injury: Even minor injuries
- Headache with Neurological Symptoms: Confusion, weakness, vision changes
- Headache Waking Child from Sleep: May indicate serious condition
Medical Evaluation
In my practice, a thorough evaluation includes:
History Taking
- Headache Pattern: Frequency, duration, timing
- Pain Characteristics: Location, quality, severity
- Associated Symptoms: Nausea, vomiting, sensitivity to light/sound
- Triggers: What seems to cause headaches
- Impact: Effect on school, activities, family life
- Family History: Headaches in family members
- Medications: Current medications and treatments tried
Physical Examination
- Neurological Exam: Check for neurological abnormalities
- Vital Signs: Blood pressure, temperature, heart rate
- Head and Neck: Check for signs of infection or other issues
- Vision: May include vision screening
- Growth: Height and weight measurements
Additional Testing
- Usually Not Needed: Most children don’t need imaging
- When Indicated: Atypical presentation, neurological symptoms, concerning features
- Imaging: MRI or CT scan only when necessary
- Other Tests: Blood tests, vision exam, or other tests as indicated
Treatment Options
From my experience, treatment depends on headache type and frequency:
Acute Treatment
- Over-the-Counter Medications: Paracetamol or ibuprofen
- Prescription Medications: For more severe headaches
- Triptans: May be used in adolescents with migraines
- Anti-Nausea Medications: If nausea is significant
- Non-Pharmacological: Rest, cold compress, relaxation
Preventive Treatment
- When Indicated: Frequent headaches (4+ per month), severe impact on life
- Medications: Various options depending on age and headache type
- Lifestyle Modifications: Regular sleep, meals, exercise, stress management
- Supplements: Magnesium, riboflavin may be considered
- Behavioral Therapies: Biofeedback, cognitive behavioral therapy
Special Considerations
- Age-Appropriate Dosing: Medications must be dosed by weight/age
- Safety: Some medications not appropriate for children
- Monitoring: Regular follow-up to assess effectiveness
- Adjustments: Treatment may need adjustment over time
Supporting Your Child
Based on my work with families, these strategies help support children:
Emotional Support
- Validation: Acknowledge that headaches are real and painful
- Reassurance: Let child know you’re there to help
- Understanding: Recognize impact on child’s life
- Patience: Recovery and management take time
- Encouragement: Celebrate improvements and efforts
Practical Support
- Treatment Plan: Help child follow treatment plan
- Prevention: Support lifestyle modifications
- Advocacy: Advocate for child at school and with healthcare providers
- Education: Help child understand their headaches
- Independence: Gradually help child manage their own headaches as they grow
Family Support
- Family Understanding: Help family members understand headaches
- Flexibility: Be flexible with family activities when needed
- Normalization: Help child feel normal despite headaches
- Support Network: Connect with other families dealing with headaches
- Self-Care: Parents need to take care of themselves too
Headache Diary for Children
In my practice, I recommend keeping a headache diary:
What to Record
- Date and Time: When headache started and ended
- Pain Intensity: Child’s rating (1-10 scale or faces scale)
- Location: Where pain was felt
- Symptoms: Nausea, vomiting, sensitivity to light/sound
- Triggers: What might have caused it
- Activities: What child was doing before onset
- Medications: What was given and effectiveness
- Sleep: Quality and duration of sleep
- Meals: What and when child ate
- School: Any school-related factors
Benefits
- Pattern Recognition: Identify triggers and patterns
- Treatment Effectiveness: Evaluate what works
- Communication: Better discussions with healthcare provider
- Empowerment: Help child understand their headaches
- Prevention: Early recognition of prodrome symptoms
Take Action Today
Based on my experience helping families, here are the next steps:
Immediate Steps
- Start a Headache Diary: Track your child’s headaches and triggers
- Identify Triggers: Look for patterns in the diary
- Implement Prevention: Regular sleep, meals, exercise, stress management
- Consult Healthcare Provider: If headaches are frequent or concerning
Long-term Planning
- Develop Treatment Plan: With healthcare provider
- Lifestyle Modifications: Support healthy habits
- School Communication: Work with school for accommodations
- Regular Follow-ups: Monitor progress and adjust treatment
- Education: Continue learning about headaches in children
Common Questions
In my practice, parents frequently ask:
-
Are headaches in children serious? Most headaches in children are not serious, but warning signs should never be ignored. Most children with headaches can be effectively managed.
-
Can stress cause headaches in children? Yes, stress is a common trigger for tension headaches in children. School pressure, social situations, and family stress can all contribute.
-
Should children take painkillers for headaches? Occasionally, over-the-counter medications can be used, but frequent use should be avoided. Always consult a doctor before regular medication use.
-
Can screen time cause headaches? Yes, excessive screen time can contribute to headaches in children through eye strain, poor posture, and reduced physical activity.
-
Will my child outgrow headaches? Some children do outgrow headaches, while others continue to have them into adulthood. Proper management can significantly improve quality of life regardless.
-
Should I be worried about my child’s headaches? Most headaches are not cause for worry, but if you’re concerned, it’s always worth discussing with a healthcare provider. Warning signs should never be ignored.
A Message of Hope
Through my years of practice, I’ve helped countless families manage headaches in children effectively. While headaches can be challenging for children and families, with proper understanding, early recognition, appropriate treatment, and lifestyle modifications, most children can achieve significant improvement in their quality of life. Remember, you’re not alone in this journey, and effective headache management is possible. Together, we can work toward better headache control and improved daily functioning for your child.
Additional Resources
- Pediatric headache support organizations
- Educational materials on headaches in children
- Healthcare provider directory
- School accommodation resources
- Support groups for families dealing with pediatric headaches
Need Professional Help?
If you or your loved one is experiencing neurological symptoms, don't hesitate to reach out. Schedule a consultation with Dr. Natasha Tipnis Shah for expert care and guidance.
Book an AppointmentSchedule Your Consultation
Take the first step towards better neurological health. Book your appointment today.
Hospital Locations
Jaslok Hospital & Research Center
K.J. Somaiya Hospital & Research Center
Somaiya Ayurvihar, Eastern Express Hwy, Sion East, Sion, Mumbai, Maharashtra 400022
24 Hours
Zynova Shalby Hospital
CTS 1900-1917, Lal Bahadur Shastri Marg, Gandhi Nagar, Kirti Vihar, Ghatkopar West, Mumbai, Maharashtra 400086
24 Hours
Heart & Vascular Superspeciality Hospital
3rd Floor, Silver Point, Lal Bahadur Shastri Marg, Kasturi Park, Maneklal Estate, Ghatkopar West, Mumbai, Maharashtra 400086
24 Hours